Summer Foot Care on Vacation
Summer Foot Care on Vacation
Summer is just around the corner, and that might mean you’re getting ready for your next vacation to the beach or another bucket-list destination. Many vacationers neglect to properly take care of their feet. Don’t let pain and discomfort get in the way of enjoying your sunny vacation.
Here is a list of tips for keeping your feet happy when traveling:
- Choose the right shoes and bring multiple pairs
When planning your vacation, understand the types of activities you’ll be doing. Will you be walking a lot? What kind of terrain will you be on? Consider these questions as you pack. It’s also important to have multiple pairs to rotate. You may be trying to pack lightly, but having a second or third pair on hand will ensure you always have a fresh pair ready to go.
- Keep blisters away
Everyone knows the feeling of an emerging “hot spot” on our feet when we don’t have proper socks or footwear on. Don’t let something preventable like a blister ruin your trip. On top of wearing clean and quality socks and shoes, consider using a blister prevention cream or tape before spending long periods of time on your feet. There are many affordable and effective travel-size products available, such as Body Glide or RockTape.
- Don’t forget sunscreen
In addition to preventing blisters from chafing, sunburn can be another source of serious discomfort. If you’re wearing sandals or open-toed shoes when the sun is out, be sure to apply sunscreen to the exposed parts of your feet and toes. It’s easy to forget to apply protection to these areas, yet your feet are one of the more vulnerable places for sunburn when exposed.
- Keep the blood flowing
If you have a long plane ride or drive to your destination, compression socks are one good way to promote good blood flow while being sedentary. Your feet and lower legs will thank you if you break up long periods of sitting with short walks, which is another way to keep a healthy blood flow and prevent discomfort. It’s also recommended to avoid crossing your legs while sitting.
The importance of happy feet can be overlooked when planning for your summer vacation. You deserve a fun and relaxing vacation, so be sure to take these easy steps to prevent pain and discomfort while traveling. If you return home from vacation with skin or nail issues around your feet, learn more about how our team of professionals can get you the relief you need.
Video: Stretches to Prevent Common Running Injuries
Video: Stretches to Prevent Common Running Injuries
Although running is a great way to stay active, many runners will deal with an injury at some point. The repetitive impact of this type of exercise can take a toll on your body, which can result in various injuries.
Let us restore your balance.
Thankfully, Balance Foot & Ankle’s Dr. Hunstman is here to give you some insight into common running injuries and how you can prevent them. In the case that professional intervention is required, our trusted team of podiatrists can help get you back on your feet with a personalized treatment plan that emphasizes a holistic approach to total wellbeing.
Four Ankle Strengthening Movements You Can Do at Home
Four Ankle Strengthening Movements You Can Do at Home
It’s no secret that our ankles play an essential role in every step we take, our ability to stay upright, and in performing almost every other physical function on a daily basis. Unfortunately, many people have weak ankles, which can often lead to injuries and chronic pain. Age, weight, footwear, overuse, trauma, and other conditions cause ankle problems. The good news is that we can take control of the health of our ankles by working to make them stronger.
Here is a list of simple, at-home exercises that will lead to healthy and strong ankles.
Movements to Strengthen Your Ankles
Before doing any exercises, make sure to warm up with a low-intensity activity such as walking or riding a stationary bike for a few minutes.
- Improve balance: Standing upright, slightly lift your left leg off the ground, shifting weight-bearing to your right leg. Hold for a few seconds and then switch legs. As you
improve, increase the amount of time you balance on each leg. - Increase range of motion: while seated, use your foot to write out the letters of the alphabet, leading with the big toe. Keep the movements small so that you are just
moving your foot and ankle and perform with each foot. - Build strength: place 20 marbles (or another small item) on the floor in front of you while seated. Use your toes to pick up and place one marble at a time into a bowl. Repeat with the other foot. A
similar exercise can be performed with a towel. Placing it in front of your feet while seated, grab the center of the towel with your toes and scrunch it towards you. Repeat
with the other foot. - Step it up a level: once you’re comfortable with the above exercises, you may be ready to progress to doing calf raises. This can be performed by standing on both legs, using a wall or chair for balance, and slowly raising one heel off the ground, then lowering it. Repeat on each leg ten times.
As always, we’re here for you. If your ankle issues persist or worsen, don’t hesitate to schedule an appointment with us today so that we can ensure you’re on the path to healthy feet and ankles.
How to Wrap an Ankle Sprain
How to Wrap an Ankle Sprain
We know that life is busy for our patients, and this can mean that even when injuries happen, you cannot always make time to see us immediately. But what can be done if you suspect you’ve injured your foot or ankle between the time it occurs and coming in for an appointment? And how can you avoid having the injury become more severe? Today we’ll discuss a common at-home care technique: wrapping an injured foot or ankle.
Why Use a Compression Wrap?
A compression wrap may help to prevent swelling, which can help to alleviate pain in the foot and ankle. It is not a brace and does provide substantial support for the ankle or prevent it from moving, however, it does give the wearer a nice reminder to go about their day in a more careful manner so as not to cause further injury.
Using a Compression Wrap Properly
Instructions
- Roll up the elastic bandage. Position your ankle at about a 90-degree angle. Begin wrapping below your toes, at the pad of your foot. Hold the loose end of the bandage at the side of your foot and wrap around, keeping the fabric taut with light tension.
- After this, wrap around the arch of the foot. Next, wrap the bandage diagonally from the bottom of the toes across the foot’s top and circle it around the ankle. Now bring the bandage diagonally across the top of the foot and under the arch in a figure-eight pattern.
- When you get to the ankle bone, wrap the bandage around the felt piece so it stays in place under the ankle bone. Continue around the ankle and foot in a figure-eight motion, moving toward the heel on the bottom and toward the calf at the top of the eight.
- The wrap should cover the entire foot and end about four inches above the ankle. Most compression wraps are self-fastening or come with clip fasteners. If not, use tape to secure the end. The wrap should be snug but should not cut off circulation to the foot.
Again, this is often a temporary solution and not a recommended therapy to address the issue. If pain or discomfort persists, you should schedule an appointment to be seen in the office at which time your doctor will evaluate and determine a proper course of action to help you back to health.
Our goal is to be sure that you are feeling your best. If that is not the case, please reach out today so that we can determine how best to help you!
Ingrown Toenails: How to Avoid Them and How to Treat Them
Ingrown Toenails: How to Avoid Them and How to Treat Them
One of the most common calls we receive at Balance Foot & Ankle has to do with an issue that can be minimized by slightly modifying the way you maintain your feet. That issue is the development of ingrown toenails. Today we’ll discuss self-care for ingrown toenails, how to spot them and when it’s time to see your doctor.
Ingrown Toenails: How Can I Avoid Them?
Practicing proper self-care for your toenails can prevent ingrown toenails and infections:
- Avoid trimming the nails too short
- Trim nails straight across rather than at an angle
- Utilize sanitary and sharp clippers and tools
- Wear shoes that fit properly
I Think I Have an Ingrown Toenail: Now What?
If you are experiencing the following symptoms you may be developing an ingrown toenail:
- Pain
- Swelling
- Redness
- A change in your skin pigmentation along the nail border
If you notice any of these changes, the most important first step is to avoid the temptation to remove the ingrown toenail on your own. This will help you to mitigate a worsening of symptoms or an infection. Instead, try soaking your feet in a warm Epsom salt soak for 15-20 minutes twice per day, applying a topical antibiotic ointment (covered by a Band-Aid), and be sure to call your doctor to schedule an appointment if necessary.
When Should I See a Doctor?
There may also be signs of pus, warmth or red streaking along the toe which may indicate an infection. Should home care fail to alleviate the symptoms or should symptoms worsen, you should schedule an appointment to be seen in the office at which time your doctor will assist in alleviating the symptoms, managing the infection and will discuss an in-office procedure if necessary.
As always, we are here to be sure you are well cared for!
Finding and Buying Shoes That Fit Properly
Finding and Buying Shoes That Fit Properly
The tell-tale signs of autumn are all around us. School bells ring once again, football games are kicking off, and just about everything comes in pumpkin spice!
As the air turns crisp, and the leaves transform into a prism of color – our wardrobes begin to change in tandem. As that favorite cozy sweater takes the place of breezy summer linens, now is the time to swap out sandals and barefoot behavior for comfortable and smart footwear choices that will have your feet feeling
supported.
After a long summer of meticulously pedicured toes in often unsupportive shoe gear, now is the time of year to give those feet much-needed support [and warmth] in boots, sneakers, clogs, etc.
Let’s talk about shoe shopping.
As I often share with my patients, there are several things to consider that go beyond the aesthetic appearance of a shoe when shopping. Whether you are shopping for shoes to get you around campus, for the office, or for weekends with friends – these tips will help keep your feet balanced.
Before you head to the shoe store, stand on a blank piece of paper and trace each foot as accurately as possible. Then take this tracing with you when shopping for shoes. Place your desired shoe on the tracing. Does the shoe cover your tracing or do you see the outline of your foot extending beyond the margins of the shoe? This can be a simple and fun way to keep yourself honest when making shoe selections. Choosing a shoe that is too narrow for your actual foot shape could set you up for future issues such as pain, calluses, blisters, ingrown toenails, and the progression of some deformities, such as bunions and hammertoes.
Next, find a reputable shoe store that can assist you in the correct shoe size, shape, and type to fit not only your feet but also your lifestyle. They will measure your feet to ensure that you are indeed selecting the correct size.
Consider shoe shopping later in the day when your feet may be a bit larger from swelling, as this is natural after a day on your feet and walking about. This will give you a better idea of the shoe size and shape that is best for you.
The last tip is to try to be reasonable and as practical as possible. Boots with a narrow toe box and narrow 4-inch heel may look beautiful, but in turn, may haunt you later down the road. Reserve those beauties for occasional outings when you know you will be sitting all night long. Go practical and comfortable for everyday wear, exercise, and casual events.
Believe me, your feet will thank you!
Callus 101: Causes, Prevention and Treatment
Callus 101: Causes, Prevention and Treatment
Foot calluses, or rough patches of skin found on the ball, heels or small toes, is a normal occurrence for most people. Caused by compression and friction, foot calluses are your body’s way of protecting the skin underneath from irritation and pressure.
Though calluses are a normal occurrence for most people, some patients are more likely to develop calluses than others. If you walk without socks, wear shoes that are too narrow for your feet or you already have a medical condition that changes the normal alignment of the bones in your feet, you’re more likely to develop calluses on your feet.
How do I prevent calluses?
Foot calluses can be prevented by wearing proper socks and shoes, including proper fitting footwear both width and lengthwise. Ensuring that worn shoes are repaired and replaced regularly can give your skin some protection from the shock of walking on hard surfaces.
How do I treat calluses?
There are numerous home remedies to reduce the appearance of calluses, though the majority of calluses can be resolved with time off of your feet. You should refrain from using sharp objects to remove or reduce calluses, as this could lead to infection.
If you’re looking to reduce the calluses on your feet, try these home remedies:
- Epsom Salts: Soaking your feet in a handful of Epsom salts in a bath or basin of warm water for ten minutes can greatly soften calluses, especially before manual exfoliation
- Padding: Adding moleskin patches or soft pads can help to protect the skin from rubbing against shoes or socks.
- Shoe inserts: Cushioned insole, arch support and heal counters can help to reduce friction on the skin, especially by moving pressure away from any problem areas.
If you are still experiencing pain from your calluses, be sure to schedule an appointment with one of our board-certified foot and ankle specialists. At Balance Foot & Ankle, we’re here to restore your balance and get you back on your feet.
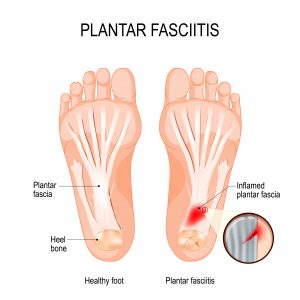
Video: Plantar Fasciitis
Video: Plantar Fasciitis
Plantar fasciitis is an inflammation of the thick piece of tissue that runs under your foot. This tissue, called the plantar fascia, can become inflamed if you have high or low arches, are wearing the wrong shoes for you, or from injury or overuse. Over time, continuing physical activities, like running and dancing, or constant standing and movement can lead to plantar fasciitis. This inflammation is one of the most common orthopedic foot complaints that can also lead to chronic plantar fasciitis. Prevention through stretching and proper shoe gear is important to keep up your everyday activities without pain.
Let us restore your balance.
If you notice the discomfort in your heels persisting, our trusted team of podiatrists at Balance Foot & Ankle can work with you to alleviate the pain by customizing a treatment plan to your lifestyle.
Daily Stretches To Prevent Plantar Fasciitis
Daily Stretches To Prevent Plantar Fasciitis
If you’re waking up with a stabbing pain in the heel of your foot with your first steps, you could be among the more than 2 million Americans with plantar fasciitis. There are many times in which discomfort from plantar fasciitis occurs, especially during long periods of walking, standing or running. Sometimes, even wearing the wrong kind of shoes can irritate your plantar fascia.
So, what is plantar fasciitis?
Plantar fasciitis is an inflammation of the thick piece of tissue that runs under your foot. This tissue, called the plantar fascia, can become inflamed if you have high or low arches, are wearing the wrong shoes for you, or from injury or overuse. Over time, continuing physical activities, like running and dancing, or constant standing and movement can lead to plantar fasciitis. This inflammation is one of the most common orthopedic foot complaints that can also lead to chronic plantar fasciitis. Prevention through stretching and proper shoe gear is important to keep up your everyday activities without pain.
How do I prevent plantar fasciitis?
Everyone should take measures to proactively prevent plantar fasciitis, and the easiest way to do this is to stretch daily. When paired with the right footwear, these five stretches can aid in prevention of plantar fasciitis.
- Toe Stretch: With your heel on the floor, use your hand to pull your big toe toward your calf. Hold this for 15-30 seconds, repeating two to four times.
- Calf Stretch: Stand facing a wall, with your hands eye level on the wall. Position one leg in front of the other, about a step apart, and bend the knee of the foot in front. You should feel a stretch in your calf on the back leg — hold this stretch for 15-30 seconds and repeat two to four times daily.
- Towel Stretch: Sitting on the floor, place a rolled-up towel under the ball of your foot, holding on to the ends. Gently pull on the ends of the towel while keeping your knee straight. Repeat this stretch for 15-30 seconds and repeat two to four times daily.
- Toe Curls with Towel: With a small towel on the floor, use your toes to curl the towel toward you. Repeat 10 times, two to four times daily.
- Ice Bottle Massage: Place a frozen can or bottle on the floor, rolling it with the arch of your foot for 10-15 minutes, two to four times daily.
Let us restore your balance.
If you notice the discomfort in your heels persisting, our trusted team of podiatrists at Balance Foot & Ankle can work with you to alleviate the pain by customizing a treatment plan to your lifestyle. Schedule your appointment today!
How To Ease Bunions Without Surgery
How To Ease Bunions Without Surgery
Bunions are bony bumps that develop on the joint of the big toe. Because they progress slowly over time, bunions may only cause occasional or mild discomfort initially. As they progress, they can begin to affect your daily routine, making it challenging to do normal tasks. The pain is usually made worse by pressure from footwear and can cause stiffness in your big toe. In more advanced cases, bunions can even cause your big toe to cross over the second toe.
Bunions may be caused by faulty mechanics, inflammatory conditions, structural deformities, trauma or genetics. Poorly fitted shoes can cause progression of bunions or exacerbation of symptoms.

How do I ease bunion pain?
While bunions cannot be reversed, there are many ways to ease bunion pain and slow the progression. You can try these easy 5 at-home remedies to ease bunion pain:
- Protect the bunion bump with moleskin or gel-filled pads when wearing shoes. This will alleviate the pressure on the joint and lessen the pain.
- Custom foot orthotics, especially those recommended by your podiatrist, paired with well-fitting shoes will allow your feet to rest comfortably and will make a day on your feet much easier.
- If you’ve just spent the day on your feet, ice, rest and elevation can relieve pain and inflammation. Alternatively, you can treat yourself to an Epsom salt soak after a long day on your feet.
- Over the counter anti-inflammatory medications, like ibuprofen, can reduce the inflammation in the affected joints.
- Finding shoes with a wide and tall toebox can relieve bunion pain— your podiatrist will be able to help you find the best pair of shoes for you.
Let us restore your balance.
If all else fails, our trusted team of board-certified podiatrists at Balance Foot & Ankle can work with you to find the right treatment for you and your lifestyle.
Schedule your appointment today!









