How you can manage everyday foot pain
How you can manage everyday foot pain
It’s one thing to have sore feet after an unusually long day of standing, walking around, or exercising more than you’re used to doing. But if low-grade foot pain and discomfort is something you experience regularly, you shouldn’t accept this as a normal part of daily life.
Being on your feet is something many of us can’t avoid. At Balance Foot & Ankle, we often hear from patients who spend long hours on their feet working in a service industry, parents running around with their children, and athletes engaging in physical activity. While every situation is unique, we find that this type of general foot pain can be significantly relieved by some simple, non-operative interventions.
Finding the right shoe for you
If you’re like a lot of people, you probably tend to shop at a large retail store or website and select a pair of shoes based on looks and price. Unfortunately, many shoes you’ll find at these retailers are either low quality or aren’t a good fit for your feet, which can cost you in the long run. While many everyday shoes appear similar, there are some key differences between each pair. There are considerations like arch support, stability, cushion, width, heel to toe drop and more that determine if a pair of shoes is right for your feet.
For example, if you have flat feet, you might benefit from a shoe with built in arch support. In some cases, you might benefit from added support through an orthotic. But the key takeaway here is that everyone’s feet are unique and it’s worth finding the type of shoes that works best for you.
Fortunately, it’s not complicated to do this. By visiting a local retailer, such as our friends at Second Sole or Arthur’s Shoe Tree, you can work with staff to measure your feet, analyze your gate, and identify any particular needs that can be addressed.
How Balance can help
In some cases, if pain persists beyond home remedies and shoe gear changes, it may be time to seek professional advice. Our board certified foot and ankle physicians and surgeons are available to take the time to better understand the underlying causes of your foot or ankle discomfort. A comprehensive exam that may include X-ray or other imaging modalities may be necessary in order to devise a treatment plan that is right for you.
Ultimately, lingering foot and ankle pain is not normal and shouldn’t be brushed off. We’re here to help – don’t hesitate to reach out and schedule an appointment today.
Let us restore your balance.
If you notice the discomfort in your heels persisting, our trusted team of podiatrists at Balance Foot & Ankle can work with you to alleviate the pain by customizing a treatment plan to your lifestyle.
Video: All About Arthritis of the Foot & Ankle With Dr. Jon Sharpe
Video: All About Arthritis of the Foot & Ankle With Dr. Jon Sharpe
As you get older, you have a higher risk of arthritis. The joint damage from this condition can cause swelling, pain, and physical changes in your feet and ankles. Learn more about this condition, possible treatment options, and when to visit a doctor with Balance podiatric surgeon Dr. Jon Sharpe!
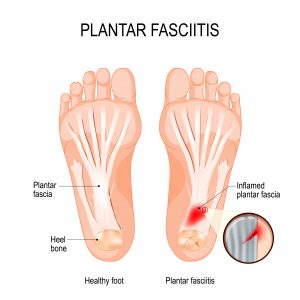
Video: Plantar Fasciitis
Video: Plantar Fasciitis
Plantar fasciitis is an inflammation of the thick piece of tissue that runs under your foot. This tissue, called the plantar fascia, can become inflamed if you have high or low arches, are wearing the wrong shoes for you, or from injury or overuse. Over time, continuing physical activities, like running and dancing, or constant standing and movement can lead to plantar fasciitis. This inflammation is one of the most common orthopedic foot complaints that can also lead to chronic plantar fasciitis. Prevention through stretching and proper shoe gear is important to keep up your everyday activities without pain.
Let us restore your balance.
If you notice the discomfort in your heels persisting, our trusted team of podiatrists at Balance Foot & Ankle can work with you to alleviate the pain by customizing a treatment plan to your lifestyle.
Daily Stretches To Prevent Plantar Fasciitis
Daily Stretches To Prevent Plantar Fasciitis
If you’re waking up with a stabbing pain in the heel of your foot with your first steps, you could be among the more than 2 million Americans with plantar fasciitis. There are many times in which discomfort from plantar fasciitis occurs, especially during long periods of walking, standing or running. Sometimes, even wearing the wrong kind of shoes can irritate your plantar fascia.
So, what is plantar fasciitis?
Plantar fasciitis is an inflammation of the thick piece of tissue that runs under your foot. This tissue, called the plantar fascia, can become inflamed if you have high or low arches, are wearing the wrong shoes for you, or from injury or overuse. Over time, continuing physical activities, like running and dancing, or constant standing and movement can lead to plantar fasciitis. This inflammation is one of the most common orthopedic foot complaints that can also lead to chronic plantar fasciitis. Prevention through stretching and proper shoe gear is important to keep up your everyday activities without pain.
How do I prevent plantar fasciitis?
Everyone should take measures to proactively prevent plantar fasciitis, and the easiest way to do this is to stretch daily. When paired with the right footwear, these five stretches can aid in prevention of plantar fasciitis.
- Toe Stretch: With your heel on the floor, use your hand to pull your big toe toward your calf. Hold this for 15-30 seconds, repeating two to four times.
- Calf Stretch: Stand facing a wall, with your hands eye level on the wall. Position one leg in front of the other, about a step apart, and bend the knee of the foot in front. You should feel a stretch in your calf on the back leg — hold this stretch for 15-30 seconds and repeat two to four times daily.
- Towel Stretch: Sitting on the floor, place a rolled-up towel under the ball of your foot, holding on to the ends. Gently pull on the ends of the towel while keeping your knee straight. Repeat this stretch for 15-30 seconds and repeat two to four times daily.
- Toe Curls with Towel: With a small towel on the floor, use your toes to curl the towel toward you. Repeat 10 times, two to four times daily.
- Ice Bottle Massage: Place a frozen can or bottle on the floor, rolling it with the arch of your foot for 10-15 minutes, two to four times daily.
Let us restore your balance.
If you notice the discomfort in your heels persisting, our trusted team of podiatrists at Balance Foot & Ankle can work with you to alleviate the pain by customizing a treatment plan to your lifestyle. Schedule your appointment today!
How To Ease Bunions Without Surgery
How To Ease Bunions Without Surgery
Bunions are bony bumps that develop on the joint of the big toe. Because they progress slowly over time, bunions may only cause occasional or mild discomfort initially. As they progress, they can begin to affect your daily routine, making it challenging to do normal tasks. The pain is usually made worse by pressure from footwear and can cause stiffness in your big toe. In more advanced cases, bunions can even cause your big toe to cross over the second toe.
Bunions may be caused by faulty mechanics, inflammatory conditions, structural deformities, trauma or genetics. Poorly fitted shoes can cause progression of bunions or exacerbation of symptoms.

How do I ease bunion pain?
While bunions cannot be reversed, there are many ways to ease bunion pain and slow the progression. You can try these easy 5 at-home remedies to ease bunion pain:
- Protect the bunion bump with moleskin or gel-filled pads when wearing shoes. This will alleviate the pressure on the joint and lessen the pain.
- Custom foot orthotics, especially those recommended by your podiatrist, paired with well-fitting shoes will allow your feet to rest comfortably and will make a day on your feet much easier.
- If you’ve just spent the day on your feet, ice, rest and elevation can relieve pain and inflammation. Alternatively, you can treat yourself to an Epsom salt soak after a long day on your feet.
- Over the counter anti-inflammatory medications, like ibuprofen, can reduce the inflammation in the affected joints.
- Finding shoes with a wide and tall toebox can relieve bunion pain— your podiatrist will be able to help you find the best pair of shoes for you.
Let us restore your balance.
If all else fails, our trusted team of board-certified podiatrists at Balance Foot & Ankle can work with you to find the right treatment for you and your lifestyle.
Schedule your appointment today!
Video: Bunions
Video: Bunions
Bunions are bony bumps that develop on the joint of the big toe. Because they progress slowly over time, bunions may only cause occasional or mild discomfort initially. As they progress, they can begin to affect your daily routine, making it challenging to do normal tasks. The pain is usually made worse by pressure from footwear and can cause stiffness in your big toe. In more advanced cases, bunions can even cause your big toe to cross over the second toe.
Let us restore your balance.
While bunions cannot be reversed, there are many ways to ease bunion pain and slow the progression. Our trusted team of podiatrists at Balance Foot & Ankle can help get you back on your feet with a personalized treatment plan that emphasizes a holistic approach to total wellbeing.
Video: Ankle Sprains
Video: Ankle Sprains
Life can be challenging when you have ankle pain. It can slow you down, or even bring you to a halt. It can make day-to-day activities, like grocery shopping or walking, an inconvenience. Find your balance and a convenient, efficient answer to alleviating ankle pain.
Let us restore your balance.
Recovery after an ankle sprain can be a long road. However, our trusted team of podiatrists at Balance Foot & Ankle can help get you back on your feet with a personalized treatment plan that emphasizes a holistic approach to total wellbeing.
Top Home Remedies To Relieve Ankle Pain
Top Home Remedies To Relieve Ankle Pain
Your ankles are the key to running, jumping and just about any physical activity that involves movement. They support your body in unimaginable ways. In fact, your ankles have the ability to carry forces equivalent to several times your body weight.
However, that’s not all your ankles can do. Your ankles bring virtue to movement — empowering vertical and horizontal motion. Simply put, ankles are the reason we can jump up and down and turn left and right.
On average Americans walk 4,000 steps a day. Over time, this may significantly utilize your ankles and cause pain. Ankle pain can certainly slow down or change your lifestyle temporarily, but, in many cases, it isn’t a permanent injury. It may simply require some special at-home attention.
Why am I experiencing ankle pain?
Often a result of an accidental fall or injury during physical activity, anyone can experience ankle pain — regardless of age. The symptoms are typically quite clear — difficulty putting weight on your ankle, swelling, redness or simply general pain originating from your ankle.
Ankle pain can come in a wide variety of imbalances, such as sprains, fractures, arthritis, tendinitis, and more. Most commonly, ankle pain is caused by a sprain, which is an injury to the ligaments connecting to your ankle bones. This is often the result of a twist or movement that overstretches or extends your ligament.
What can I do at home as a remedy for ankle pain?
As soon as you notice ankle pain, or have an injury that strains your ankle, take preventative measures to help alleviate any lasting pain or swelling. That way you can get back on your feet as soon as possible.
To bring balance and remedy your ankle, just remember RICE — Rest, Ice, Compress and Elevate — a simple and established at-home method for ankle pain relief and recovery.
- Rest to protect your ankles and be sure to stop any activity that causes further agitation.
- Ice to reduce pain and swelling, using a cold pack at 10 to 20-minute intervals.
- Compress to decrease swelling, wrapping a bandage around your ankle.
- Elevate to alleviate pain and swelling, lifting your foot and applying an ice pack.
As soon as your ankle’s soreness and pain subside, make sure to stretch daily before attempting to return to normal activities and exercises.
We’re here to help you find your balance
So, when should you visit a podiatrist for your ankle pain?
If the RICE method and over-the-counter pain relievers do not seem to be helping, there may be other solutions that can only be provided by a podiatrist that understands your unique biomechanics. In some cases, custom orthotics can put you on the right path to recovery. However, everyone’s unique feet and ankles require innovative solutions that fit their lifestyle and body. So, it’s best to schedule an appointment directly with a podiatrist for foot and ankle pain relief.
From medical and surgical appointments to aesthetics and wellness, Balance Foot & Ankle’s well-rounded and comprehensive approach to foot and ankle treatment fosters an environment of excellence, hospitality and compassion within a contemporary yet warm setting.
Experience a balanced approach to total wellbeing at a location convenient for you.
Keys To Achieving Better Outcomes With Shin Splints
Keys To Achieving Better Outcomes With Shin Splints
Source: PodiatryToday
“I love the academic challenge that shin splints pose to figure out what is wrong and what muscle or tendon is contributing to the issue at hand. I break down shin splints into medial, lateral, anterior and posterior shin splints.” – Richard Blake DPM
Medial shin splints involve the posterior tibial tendon, flexor hallucis longus tendon or the flexor digitorum longus tendon.
Lateral shin splints involve the peroneus longus tendon or the peroneus brevis tendon.
Anterior shin splints involve the anterior tibial muscle, extensor hallucis longus tendon, extensor digitorum longus tendon or the peroneus tertius tendon.
Posterior shin splints involve the gastrocnemius muscle or the soleus muscle.
The actual definition of shin splints is pain between the ankle and the knee. There are a lot of structures with potential involvement that are important to consider when treating these symptoms.
When we treat shin splints, we can simply emphasize activity modification, some ice, general leg strengthening, and cross training, and most patients will do fine. However, if we treat shin splints with a little more zest, we can prevent reoccurrence. This may mean a longer running career for an athlete. For the patient who does not respond to simple measures, he or she could have compartment syndrome or tibial/fibular stress fractures. Muscle testing sometimes helps but most cases of shin splints are associated with muscle fatiguing when athletes get tired. This is hard to test in the office when the patient is rested although I normally have patients intensely work out or work out to the threshold of pain before their appointment late in the day. One muscle testing principle is to test the muscle in two basic positions: one where the patient has the advantage and one where the examiner has the advantage. When you test a muscle with the tendon shortened, you give the patient the advantage. When you test a muscle with the tendon stretched out, you (the examiner) have the advantage. At times, it is testing with the tendon stretched out that you find the weakness. You can pick up subtle weaknesses this way.
A thorough understanding of shin splints starts with classification as one of these four types and then delving into the function of the muscles. It is important to identify how the patient may have overused that muscle or muscle group. For the purposes of this blog, I will focus on medial shin splints.
If the patient presents with medial shin splints, we need to look for overuse with the posterior tibial, flexor digitorum longus and flexor hallucis longus muscles. These muscles have many functions but let us look at what they do at the ankle.
Since they all arise from the deep compartment, these muscles are ankle plantarflexors and ankle invertors. What is the primary ankle plantarflexor? That is the Achilles tendon but anything that makes the Achilles tendon weak can cause a patient to overuse one of the three muscles causing medial shin splints as they try to help the Achilles tendon perform its job. Typical weakness in the Achilles may stem from simple fatigue in doing a new sport or from adding hills to a running program. However, force-length physics considers an over-stretched Achilles or excessively tight Achilles weak. With the recent craze of zero-drop shoes, I now see more Achilles strain problems, the resultant weakness and then development of anterior or medial shin splints.
The ankle inverter function is probably the more common cause of medial shin splints. What taxes the inversion strength of these muscles? Excessive pronation can cause these three muscles to fatigue and strain as they attempt to decelerate the pronation. As the arch collapses in pronation, all three of these tendons can strain, but this is especially the case with posterior tibial tendon as the primary decelerator of rearfoot pronation at heel contact.
What are some of the causes of excessive pronation? Running itself with landing on the lateral side of the heel will cause two to four times more pronation than walking in many runners.1 Another one of the common causes of severe foot pronation is equinus. This tightness can be the cause of posterior shin splints but also anterior and medial shin splints. This is why a complete understanding of Achilles strength and flexibility is crucial. If the Achilles is tight, it is harder for the anterior extensors to dorsiflex the foot (thus causing anterior shin splints). If the Achilles is tight, the foot can pronate and the arch collapses (medial shin splints), both putting strain on the functions of the deep posterior compartment. If the Achilles is tight, the forefoot is forcibly loaded by ground reactive force, making it difficult to bend the toes in propulsion. Stress influences the long flexors (medial shin splints) and long extensors (anterior shin splints).
In Conclusion
So when a patient comes into my office with shin splints, I need to see what type he or she has (medial, lateral, anterior, or posterior) and determine what the patient did wrong other than add a new sport. I need to check for excessive pronation. I watch him or her run since running and walking for a patient can be totally the same or different. I need to measure for Achilles tightness or over-flexibility. I need the patient to wear his or her normal running shoes. If the patient is a pronator, I also want to categorize this as mild, moderate or severe so I can determine what level of support to offer in my treatment to lower the tissue stress threshold and allow healing.
This is where podiatry usually excels since proper shoes, custom or over-the-counter insoles, appropriate strengthening exercises and taping can speed up rehabilitation and prevent recurrence. In a future blog, I will discuss stress fractures, anterior and lateral shin splints, and other general rules.
Dr. Blake is in practice at the Center for Sports Medicine, which is affiliated with St. Francis Memorial Hospital in San Francisco. He is a past president of the American Academy of Podiatric Sports Medicine. Dr. Blake is the author of the recently published book, “The Inverted Orthotic Technique: A Process Of Foot Stabilization For Pronated Feet,” which is available at www.bookbaby.com.
Editor’s note: This blog originally appeared at www.drblakeshealingsole.com. It is adapted on PodiatryToday.com with permission from the author.
Reference
- Williams 3rd DS, McClay Davis I, Baitch SP. Effect of inverted orthoses on lower extremity mechanics for runners. Med Sci Sports Exerc. 2003;35(12):260-268.
What Is A Podiatrist And When Should You Visit One?
What Is A Podiatrist And When Should You Visit One?
Your feet are complex anatomical structures that are critical to your overall health and well-being. They stabilize you as you walk and stand, absorb shock when you jump and land, and propel you into motion when you push off for a jog. As such, if an injury occurs or treatment is needed, your feet require and deserve expert care from a DPM (doctor of podiatric medicine).
What is a podiatrist?
Podiatrists (DPMs) are medical specialists focused on treating problems that affect the foot, ankle and related structures of the leg. They can also treat foot-related injuries and complications that result from ongoing health issues, like diabetes.
Before practicing, podiatrists must complete four years of training in a podiatric medical school followed by three years of hospital residency training. In some cases, additional fellowship training is obtained for further advancements in specialty training. Additionally, to further advance their expertise, some podiatrists may also earn board certification from the American Board of Foot and Ankle Surgery and the American Board of Podiatric Medicine.
When should you visit a podiatrist?
Your feet keep your life’s journey in motion. In fact, according to the American Podiatric Medical Association (APMA), by the time you’re 50, you’ll have walked 75,000 miles on your feet. Don’t let foot or ankle pain slow you down on your journey. Instead, visit a podiatrist to treat pains affecting your feet, like:
- Fractures and sprains
- Arthritis
- Skin and nail disorders
- Diabetes
- Heel pain
- Bunions and hammertoes
Experience a Balanced Approach to Total Wellbeing
From medical and surgical appointments to aesthetics and wellness, Balance Foot & Ankle’s well-rounded and comprehensive approach to foot and ankle treatment fosters an environment of excellence, hospitality and compassion within a contemporary yet warm setting.
Take a virtual tour of our Lakewood clinic here.
Ensuring superior standards, products and care at Balance’s clinic, the staff of experienced specialists and highly trained surgeons prioritize building relationships with patients, clients and community. In this way, the Balance staff is able to design personalized treatment plans that address each individual’s unique set of needs whilst emphasizing a holistic approach rooted in education, health and wellness.
Experience a balanced approach to total wellbeing. Schedule your appointment today!